Cold and Heat Therapy in Shoulder Rehabilitation
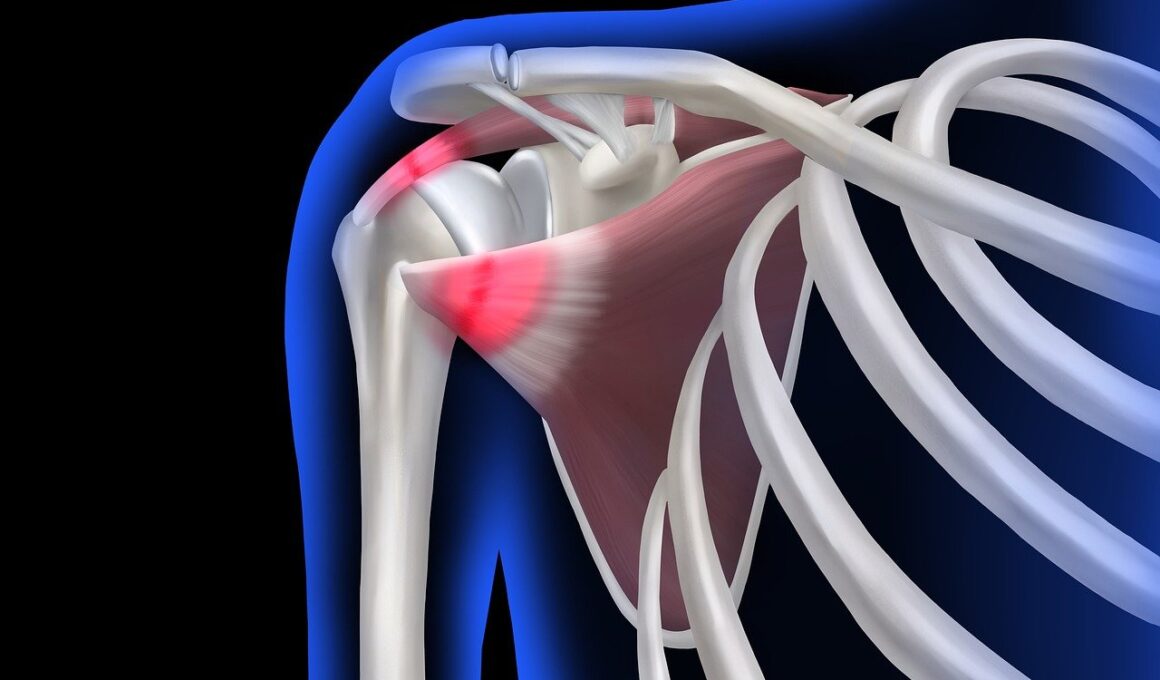
Rehabilitation for shoulder injuries often involves various therapeutic strategies, among which cold and heat therapy play crucial roles. Cold therapy, also known as cryotherapy, is essential during the initial phase of injury. It minimizes swelling, reduces inflammation, and numbs sharp pain due to acute injuries. The application of ice packs or cold compresses for approximately 15 to 20 minutes several times a day can prevent excess inflammation and facilitate the healing process. Additionally, cold therapy slows blood flow to the affected area, helping to mitigate pain and decrease muscle spasms. Patients often report significant relief from acute injuries, including strains or sprains within the shoulder. However, this method should not be overused and is ideally applied within the first 48 hours of an injury. Following this, transitioning to heat therapy aids in recovery. Heat therapy promotes blood circulation, relaxes tight muscles, and provides comfort, making it an effective method in the later stages of shoulder rehabilitation. It’s essential to alternate between methods as needed for optimal recovery, ensuring that rehabilitation remains effective and safe. Engaging in discussions with healthcare providers about the best expressions is very important.
Understanding the physiological effects of cold and heat therapy informs their appropriate application within shoulder rehabilitation. Cold therapy constricts blood vessels, causing a decrease in metabolic activity which limits the extent of inflammatory responses in the injured tissues. This process is beneficial immediately after an injury when acute inflammation is prominent. Conversely, heat therapy expands blood vessels, enhancing the blood flow to the muscles and tissues. This increased circulation allows nutrients and oxygen to reach damaged areas more efficiently, thereby promoting healing. It’s vital for patients to apply heat therapy to the shoulder after the initial swelling subsides, typically after 48 hours. Another advantage of heat therapy is its ability to alleviate stiffness associated with shoulder injuries allowing greater range of motion and flexibility during rehabilitation exercises. Certain individuals may experience conflicting results with either therapy, emphasizing the necessity of personalized treatment plans. Healthcare professionals often assess the specific circumstances surrounding a shoulder injury to recommend a tailored rehabilitation routine. Regularly monitoring responses to therapy will help determine optimal durations and frequencies of applications for both cold and heat modalities. Together, these treatments can significantly enhance recovery outcomes for shoulder injuries.
Implementing Cold Therapy in Your Routine
Effective implementation of cold therapy during the rehabilitation of shoulder injuries is essential. Patients are encouraged to begin with an assessment of their pain level, ensuring it is appropriate to use cold therapy as an initial treatment approach. This method is particularly effective within the first two days after injury to minimize swelling and pain. A common technique involves applying ice directly to the injured area using an ice pack, a specialized cold wrap, or even frozen peas wrapped in a towel. It is crucial to avoid direct contact of ice with the skin to prevent frostbite, allowing a thin layer of fabric as a barrier. Patients should set a timer for 15 to 20 minutes, allowing the skin to return to normal temperature before the next application. Additionally, integrating cold therapy into daily routines can enhance comfort by addressing pain proactively. Some may prefer utilizing cold therapy during physical therapy sessions to ensure immediate relief and allow for improved participation in rehabilitation exercises. With proper guidance, individuals can significantly benefit from precise cold therapy techniques as part of their overall recovery strategy.
Once the immediate phase of recovery has passed, incorporating heat therapy becomes increasingly beneficial. For shoulder rehabilitation, applying heat can promote enhanced relaxation and prepare the muscles for movement. Moist heat, such as a warm towel or heating pad, is typically favored as it penetrates deeper into muscles and provides longer-lasting comfort. For patients, it’s advisable to initiate heat therapy before exercising to increase blood flow and elasticity within the surrounding tissues. Maintaining the heat application for roughly 15 to 20 minutes can help reduce stiffness and improve mobility. Likewise, patients recovering from surgery found benefits through sessions of heat applications to minimize discomfort effectively. Another method includes taking warm showers or baths, which can also promote relaxation and prepare the muscles for any rehabilitation routine. It’s essential to monitor the temperature closely when using heat applications to avoid burns while ensuring maximum comfort. As with cold therapy, patients should communicate with their healthcare providers about incorporating heat therapy into their rehabilitation plans. Correct timing and proper application are crucial for ensuring the effectiveness of this therapeutic method.
Combining Cold and Heat Therapy
Making optimal use of both cold and heat therapy during rehabilitation is essential for successful recovery from shoulder injuries. The most effective approach often involves alternating between cold and heat applications, which can provide therapeutic benefits over various recovery stages. Initially, following an acute injury, patients are recommended to begin with cold therapy to manage swelling and pain. Once inflammation decreases and the shoulder begins healing, transitioning to heat therapy can greatly enhance recovery. This is due to the gradual improvement in blood flow and relaxation within the muscles that heat applications provide. Effective guidance from healthcare providers can help determine specific intervals between cold and heat applications to achieve the best outcomes. Consider keeping a consistent schedule of alternating therapy techniques, ensuring that the shoulder receives both treatments at appropriate times. Furthermore, combining both therapies alongside gentle exercises can lead to more significant improvements in mobility and function. Ensuring a thorough understanding of when to apply each modality plays a critical role in customizing rehabilitation programs effectively tailored to individual needs.
Overall, understanding both the benefits and limits of cold and heat therapy is particularly vital in the rehabilitation of shoulder injuries. Cold therapy is effective primarily in managing acute symptoms and preventing swelling immediately after injury. It is beneficial during the first two days following injury as part of the guided recovery process. While cold applications address inflammation, heat therapy provides a valuable method for alleviating persistent discomfort associated with stiff muscles later on. Combining therapies effectively can yield improved ranges of motion throughout rehabilitation and significantly enhance the quality and speed of recovery. To optimize the results of each therapy, individuals should adhere to safety guidelines and recommendations from their healthcare providers. Learning effective techniques for both therapies will contribute to informed decisions during rehabilitation journeys. Also, incorporating both modalities into individualized recovery routines can pave the way to greater success in restoring shoulder function. Engaging in conversations with physiotherapists can help reinforce understanding and design tailored rehabilitation programs that combine both techniques for maximum efficacy. Investing effort and time in personalized rehabilitation will yield improvements in experiences and outcomes.
Conclusion: The Path Forward
In conclusion, effective rehabilitation from shoulder injuries is multifaceted, leveraging methods such as cold and heat therapy. Each modality serves unique purposes within different recovery stages and can significantly enhance the healing process when used appropriately. Understanding how to implement these therapies safely and effectively represents a significant step towards recovery. By actively engaging in rehabilitation, including adhering to recommended therapies and exercises, individuals enhance their healing potential. Furthermore, integrating cold and heat therapy into daily routines empowers patients, allowing them to take charge of their recovery journey. Variability in patient experiences emphasizes the importance of personalized approaches tailored to individual needs. Regular communication with healthcare professionals supports the continual refinement of therapeutic strategies, ensuring optimal results. Progress monitoring is also essential as it underscores improvements, motivating individuals to strive for an active lifestyle post-rehabilitation. A comprehensive understanding of cold and heat therapy within shoulder injury rehabilitation can pave the way for successful return to activities. Therefore, patients are encouraged to actively involve themselves in their recovery and engage in explorative discussions about therapeutic options during rehabilitation.
Overall, understanding both the benefits and limits of cold and heat therapy is particularly vital in the rehabilitation of shoulder injuries. Cold therapy is effective primarily in managing acute symptoms and preventing swelling immediately after injury. It is beneficial during the first two days following injury as part of the guided recovery process. While cold applications address inflammation, heat therapy provides a valuable method for alleviating persistent discomfort associated with stiff muscles later on. Combining therapies effectively can yield improved ranges of motion throughout rehabilitation and significantly enhance the quality and speed of recovery. To optimize the results of each therapy, individuals should adhere to safety guidelines and recommendations from their healthcare providers. Learning effective techniques for both therapies will contribute to informed decisions during rehabilitation journeys. Also, incorporating both modalities into individualized recovery routines can pave the way to greater success in restoring shoulder function. Engaging in conversations with physiotherapists can help reinforce understanding and design tailored rehabilitation programs that combine both techniques for maximum efficacy. Investing effort and time in personalized rehabilitation will yield improvements in experiences and outcomes.