Hormonal Adaptations to Long-Term Intermittent Fasting Regimens
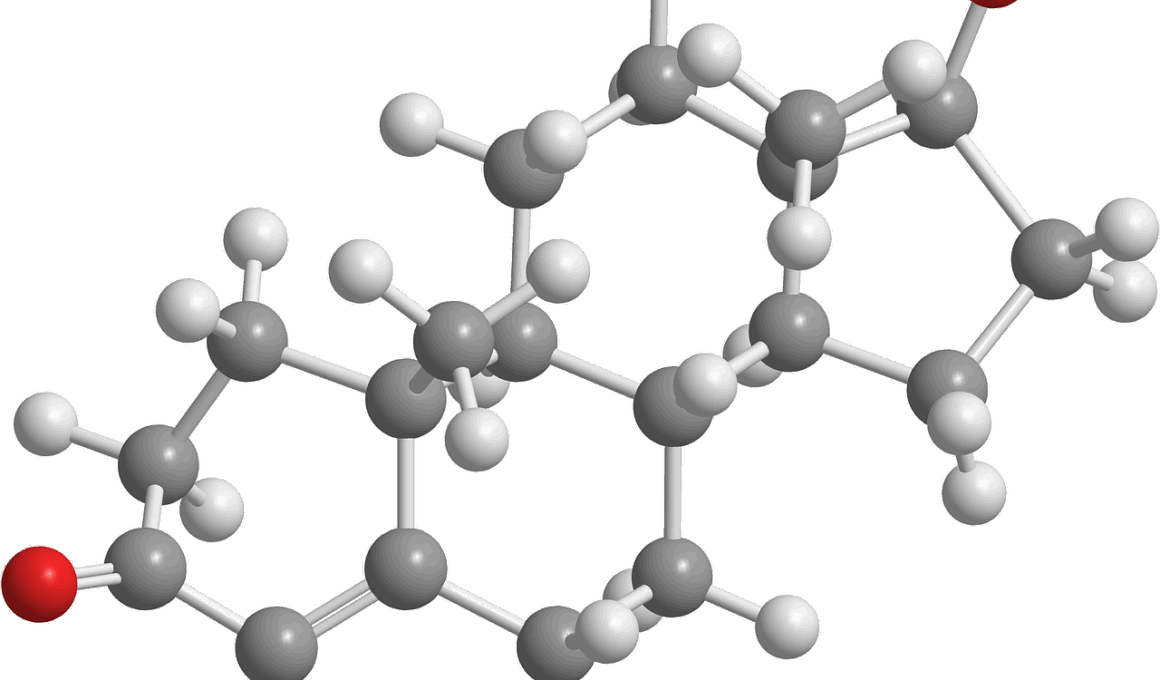
Intermittent fasting (IF) offers a unique approach to dietary regimens, shaping not only meal timing but also hormonal activity in the body. This diet, which alternates between periods of eating and fasting, has garnered significant attention due to its potential health benefits. Various studies suggest that IF can lead to hormonal adaptations that may confer advantages in weight management and metabolic health. One of the most notable hormones affected by intermittent fasting is insulin, a key regulator of blood sugar levels. During fasting periods, insulin levels typically drop, which prompts the body to burn fat for energy. This drop in insulin is essential for fat loss, as it allows cells to access stored fat more efficiently. Moreover, fasting promotes an increase in glucagon, another hormone that works alongside insulin, emphasizing the body’s ability to tap into its fat reserves. The interplay between fasting and these hormones offers insights into how our bodies can adapt hormonally and metabolically over time with long-term intermittent fasting. By understanding these changes, individuals can make informed decisions about their fasting practices and potential health outcomes.
Alongside insulin and glucagon, intermittent fasting also significantly influences growth hormone (GH) levels. This hormone plays a crucial role in metabolism, muscle growth, and fat burning. Notably, fasting has been shown to increase GH secretion by as much as five-fold, especially in response to short-term fasting periods. The elevation in growth hormone can have profound effects on body composition, promoting lean muscle retention while facilitating fat loss. This aspect is particularly advantageous for individuals looking to maintain or build muscle mass while losing weight. Additionally, growth hormone has positive effects on overall health, as it helps in tissue repair and regeneration. Fasting enhances not only GH’s secretion but also its overall effectiveness. With these hormonal adaptations, individuals engaged in long-term intermittent fasting can see more significant improvements in physical performance and body composition outcomes. It’s essential to note that these benefits can vary based on individual factors, such as age, sex, and baseline health status. Therefore, personalized approaches to intermittent fasting may be necessary to optimize hormonal balance and ensure sustainable health improvements.
Effects on Stress Hormones
Another critical aspect of intermittent fasting involves its impact on cortisol, often referred to as the stress hormone. During fasting periods, cortisol helps mobilize energy by breaking down glycogen and fat stores for immediate use. However, an excess of cortisol, especially for prolonged periods, can lead to health issues such as weight gain, fatigue, and high blood pressure. Therefore, understanding how fasting alters cortisol levels is vital. Research indicates that short intervals of fasting may elevate cortisol levels, which is naturally counterbalanced by the body’s adaptability over time. In contrast, long-term adherence to IF can stabilize cortisol production, suggesting a balance where the body becomes more efficient at managing stress levels. Normalizing cortisol is fundamental for maintaining healthy metabolic functions and reducing the risk of stress-related ailments. Thus, while intermittent fasting can initially increase stress hormones, a well-structured long-term regimen may adjust hormone profiles favorably. When combined with adequate nutrition during eating windows, this can enhance overall health outcomes and improve resilience against stress.
Hormones Related to Appetite Control
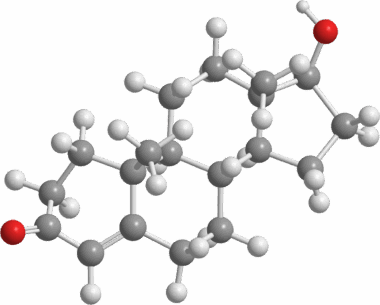
Intermittent fasting also plays a significant role in regulating appetite-related hormones, namely ghrelin and leptin. Ghrelin, known as the hunger hormone, is secreted primarily in the stomach and signals hunger to the brain, prompting food intake. In contrast, leptin is produced by fat cells and signals satiety, helping the body recognize when to stop eating. Research shows that intermittent fasting can help regulate the balance of these hormones, decreasing ghrelin levels while increasing leptin sensitivity. This mechanism is essential for managing hunger and promotes healthier eating patterns. Furthermore, improved leptin sensitivity can lead to better metabolic health, as it helps prevent overeating and supports energy balance. As individuals adapt to intermittent fasting, the modifications in ghrelin and leptin can enhance overall appetite control, making it easier to adhere to dietary plans. This shift not only aids weight management goals but also contributes to more stable energy levels throughout the day. Ultimately, the hormonal changes associated with intermittent fasting offer valuable insights into long-term dietary success.
Intermittent fasting is also associated with an increase in neuroprotective factors, among which BDNF (Brain-Derived Neurotrophic Factor) plays a significant role. BDNF is crucial for brain health and function, promoting the survival of neurons and facilitating learning and memory processes. Research suggests that IF may elevate BDNF levels, driven by the fasting state’s metabolic shifts and stress response. By enhancing BDNF production, intermittent fasting may provide protective effects against neurodegenerative conditions. This hormonal change adds another layer to the benefits of intermittent fasting, illustrating its potential protective effects on cognitive health as individuals age. However, the relationship between BDNF and fasting also suggests that adherence to fasting protocols should be monitored and adjusted to maximize benefits without inducing excessive stress. For many individuals, incorporating intermittent fasting could significantly contribute to improved mental clarity and cognitive function, alongside physical health improvements. Exploring the interplay between intermittent fasting and neuroplasticity highlights the broader implications of diet on overall health.
As we delve deeper into the long-term effects of intermittent fasting, it’s essential to consider its implications on thyroid hormones. The thyroid gland is pivotal in regulating metabolism, and any hormonal fluctuations can greatly influence energy levels and weight management. Studies indicate that intermittent fasting can lead to a decrease in thyroid hormone levels, particularly T3. While this might seem counterintuitive, some experts propose that this decline is a protective mechanism in response to caloric restriction. When the body senses a decrease in energy intake over time, it may lower metabolic demands to preserve energy and maintain body weight. However, a significant reduction in thyroid hormones can lead to unwanted effects, such as fatigue and cold intolerance. It is crucial for those pursuing intermittent fasting to monitor their thyroid function and consult with healthcare professionals. Adjustments in diet, fasting duration, or nutrient intake can be necessary to ensure hormonal balance is maintained while reaping the benefits of intermittent fasting. This highlights the importance of a well-rounded approach to dietary changes.
Long-Term Considerations for Hormonal Health
As intermittent fasting gains popularity, it’s crucial to recognize individual variation in response to these dietary strategies. Hormonal adaptations to long-term intermittent fasting should be personalized and monitored, as each person’s body has unique needs. Factors such as age, gender, lifestyle, and existing health conditions significantly influence how fasting and hormone levels interact. Understanding these nuances can empower individuals to design a fasting regimen that complements their physiological conditions. It’s advisable to incorporate a variety of nutrient-dense foods during eating windows to mitigate potential nutrient deficiencies. This attention to dietary quality can enhance the benefits of intermittent fasting while supporting overall hormonal balance. Additionally, staying hydrated and managing stress levels through lifestyle practices can further promote hormonal health. Regular monitoring and adjustments based on personal experiences and health markers will ensure the fasting regimen is beneficial over time. Overall, hormonal adaptations highlight the intricate relationship between diet and metabolic health, paving the way for more personalized and effective approaches to intermittent fasting.
In conclusion, intermittent fasting brings about significant hormonal adaptations that can positively impact health over the long term. From improvements in insulin sensitivity to increased growth hormone and stable appetite regulation, these changes promote an optimal metabolic state. However, the influence of intermittent fasting on cortisol and thyroid hormones underscores the importance of cautious implementation. Personal variations in hormonal responses necessitate a customized approach to fasting regimens. By balancing intermittent fasting with appropriate dietary choices and lifestyle adaptations, individuals can harness its benefits while minimizing potential risks. It’s essential to engage in self-monitoring and possibly medical supervision during prolonged fasting protocols. This awareness will aid in identifying any adverse effects and promote overall well-being. Educating oneself is crucial when embarking on an intermittent fasting journey, as understanding hormonal dynamics empowers better decision-making. Ultimately, the goal should always be sustainable health improvements and enhanced well-being through evidence-based practices. Through individualized strategies that account for hormonal health, intermittent fasting can become a powerful tool for achieving long-term wellness and vitality.