The Impact of Illness on Exercise Routines for Diabetics
For individuals managing diabetes, the importance of regular exercise cannot be overstated. Regular physical activity plays a crucial role in maintaining blood sugar levels, improving cardiovascular health, and enhancing overall well-being. However, when illness strikes, whether it’s a common cold or something more severe, establishing a workout routine can become challenging. During recovery, body strength diminishes, and energy levels plummet, making it hard to stick to exercise regimes. Moreover, illness often leads to fluctuating blood sugar levels, necessitating careful monitoring for those with diabetes. Therefore, it is essential to adapt fitness routines to maintain health without overexerting yourself. Consulting healthcare providers can yield personalized recommendations to navigate exercise adjustments during illness. Doctors may suggest lighter activities such as stretching or walking, which are less taxing on the body while still beneficial. Additionally, understanding the signs when to pause physical activity entirely is vital to prevent complications. Adapting to these changes can help diabetics maintain positive health outcomes despite the challenges that illness presents. Hence, awareness and preparation are instrumental in successfully managing exercise routines during times of illness for diabetics.
When dealing with illness, diabetics face unique challenges regarding their usual exercise habits. During periods of sickness, energy levels tend to decrease significantly. This can lead to a lack of motivation, which may result in fewer workouts. Adapting to this situation is crucial. One way to adjust is by altering the type of exercise performed. For example, instead of more rigorous activities, it might be beneficial to engage in lighter forms of exercise, like yoga or Tai Chi. These low-impact activities can enhance flexibility and boost mood without requiring substantial energy. It’s also essential to listen to one’s body. Chronic fatigue or discomfort might signal the need for rest. Establishing a routine that incorporates both rest and light movement can be advantageous to help maintain a balance. Keeping track of blood sugar levels is another critical aspect to consider when ill. Exercise can affect blood glucose differently depending on an individual’s condition. Therefore, consulting medical professionals regarding exercise during illness is recommended to ensure safety and efficacy in managing diabetes effectively. Finding a reasonable balance during recovery ensures that positive health outcomes continue even when the unexpected arises.
Creating a Flexible Workout Plan
Flexibility in a workout plan is essential, especially for diabetics during phases of illness or recovery. A rigid program may lead to frustration and feelings of defeat, whereas allowing for adjustments can contribute to sustaining healthy habits. Considering a mix of activities may offer a refreshing approach. For instance, incorporating various types of exercises like swimming, walking, or light home workouts can keep the routine enjoyable while facilitating a stress-free environment for recovery. It’s also beneficial to set realistic expectations. Rather than aiming for strenuous workouts, setting attainable goals based on energy levels can enhance motivation. Additionally, engaging with groups or friends for light exercise can simultaneously provide social support and accountability. Tracking progress, even in small increments, can foster a sense of achievement. Simple metrics might include the duration of a walk or the number of stretches done during a session. This can keep spirits high, encouraging a positive mindset even when feeling under the weather. By creating adaptable routines, individuals can support their health better while managing diabetes challenges that illnesses often bring.
Recognizing the signs that indicate a need to postpone exercise is vital for those with diabetes, especially during illness. Some common symptoms, like increased fatigue, sore muscles, or fever, signal that the body requires additional rest. Ignoring these signs can lead to overstress, which may aggravate health conditions and hinder recovery. It’s essential to differentiate between general discomfort from exercise adaptation and true signs of illness. During illness, blood sugar levels may fluctuate unpredictably, making physical activity potentially risky without proper monitoring. Using continuous glucose monitors or frequent blood checks can aid diabetics in understanding their body’s status during these times. Moreover, staying hydrated plays a pivotal role in maintaining optimal health and energy levels. Proper hydration assists in digestion and can positively influence blood sugar regulation, which is especially critical during illness. If possible, opting for lightweight activities like gentle stretching or short walks can help maintain some level of physical engagement without overexerting. Prioritizing proper nutrition is also imperative during sickness. Nutrient-dense foods support recovery and overall health, thereby maintaining stability in blood sugar levels even during challenging times.
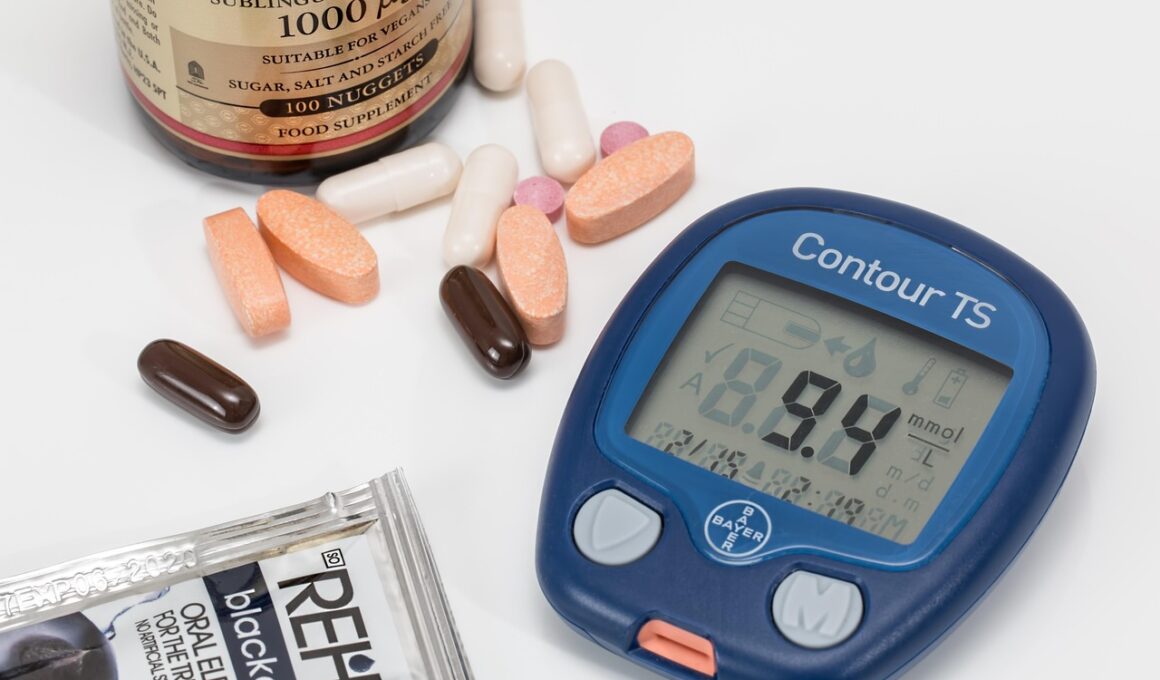
Importance of Monitoring Blood Sugar Levels
Monitoring blood sugar levels is essential for diabetics, particularly during illness when body stress increases. Health problems can disrupt the balance of glucose, resulting in unexpected highs or lows. As illness affects appetite, energy expenditure changes may occur, complicating blood sugar management. Constantly checking glucose levels allows for timely adjustments in diet, insulin, and physical activity. If elevated fasting blood sugar readings occur, it may indicate that exercise should be moderated. Conversely, if glucose levels drop significantly with illness or after medication, it can necessitate immediate action, like consuming a quick source of carbohydrates. This highlights the necessity of maintaining a reliable method of logging health metrics. Regular check-ins promote informed decisions regarding fitness ambitions and overall wellbeing. Furthermore, understanding the body’s signals during health fluctuations can deliver valuable insights into tailoring exercise plans. Notably, each individual’s condition is unique, so adapting these practices requires ongoing communication with healthcare professionals for the best outcomes. Prioritizing blood sugar monitoring during illness ensures that individuals with diabetes can navigate recovery without compromising their health or safety.
Preparing for potential setbacks due to illness requires strategizing. Being proactive can mitigate the psychological impact of missing workout sessions. Establishing an ‘exercise maintenance plan’ is beneficial and can include light exercises that aid in maintaining muscle tone without causing fatigue. Activities such as light resistance band workouts, Pilates, or mindful movements create an option without overwhelming the person affected by illness. Emphasizing a mindset of acceptance is also crucial. Accepting that rest is sometimes necessary fosters emotional resilience, preventing potential feelings of guilt for not adhering to a strict workout plan. Journaling thoughts regarding progress and emotional responses can create awareness of how expectations align with reality. Additionally, plans can include alternative routines for when recovery time is needed. Having several activities, including leisure walks or at-home workouts, can foster a sense of normalcy. By planning for setbacks and crafting adaptable routines, individuals can empower themselves to maintain health without feeling discouraged when facing illness. This strategy can lead to greater adjustments in lifestyle practices, nurturing an environment where health and wellness can flourish regardless of temporary health issues.
Establishing Support Systems
Creating and leveraging support systems can significantly influence the ability of diabetics to maintain exercise routines during illness. Friends, family, or support groups play vital roles in encouraging and providing motivation during times of need. When feeling unwell, having someone to share experiences and workouts with can elevate spirits and lend a sense of accountability. In some cases, finding an exercise buddy allows the individual to engage in modified workouts while establishing camaraderie. Additionally, health professionals can offer tailored fitness recommendations at lower energy levels as wellness continues through illness. By maintaining contact with healthcare providers, patients can receive guidance on adapting their routines as their condition evolves. Mobile applications and online platforms also offer a myriad of resources, providing community support through virtual channels. Utilizing these advancements can create an enriching environment where sharing experiences and advice helps others face similar challenges. Support systems can help promote resilience and motivation in maintaining healthy habits, especially during illness. Thus, fostering these connections promotes an overall paradigm of collective empathy and understanding, benefiting individuals with diabetes facing exercise challenges due to illness.
In conclusion, understanding and implementing the nuances of exercise routines during illness is vital for those managing diabetes. Health setbacks can lead to emotional turmoil, particularly when exercise regimens are disrupted. Flexibility is crucial; adapting workouts alongside regular monitoring of blood sugar levels encourages a health-positive environment. Setting realistic goals, engaging in leisurely activities, and maintaining open communication with healthcare professionals all play pivotal roles in navigating health challenges effectively. Recognizing when to pause or modify workouts ensures safety and well-being remains the priority during recovery phases. Above all, establishing support systems manifests positivity, facilitating shared experiences and accountability. Connecting with friends, family, or professional support fosters a compassionate approach to health management. This multi-faceted approach not only assists in managing diabetes but also promotes emotional well-being during trying times. By integrating these strategies, individuals living with diabetes can continue thriving despite the challenges that illness may pose. Thus, creating empowerment and resilience is essential in adopting and maintaining physical activity in daily life, highlighting that organized, supportive environments greatly enhance the path toward health stability while navigating the path of illnesses.