Exercise Prescription for Older Adults: Strategies and Benefits
Exercise is crucial for older adults, offering numerous physical and mental advantages. Regular physical activity can significantly enhance overall well-being, mobility, and independence. However, creating an effective exercise program for older adults involves careful consideration of individual capabilities and health conditions. Exercise prescriptions should be tailored to address specific needs, taking into account existing medical issues, functional status, and personal goals. Benefits of a customized exercise plan include improved cardiovascular health, stronger muscles, better balance, and increased flexibility. Older adults can greatly benefit from low-impact activities such as walking, swimming, or cycling, as these exercises minimize stress on joints. It is important to gradually increase activity levels while ensuring safety through proper techniques and supervision if necessary. Furthermore, encouraging participation in group activities fosters social interaction and motivation, which can positively affect adherence to the program. In prescribing exercise, healthcare professionals should aim to engage older adults in a variety of activities that they enjoy, promoting a positive attitude toward fitness. Overall, a well-structured exercise prescription contributes to enhancing the quality of life, allowing older adults to maintain their independence as they age.
Challenges in Exercise Prescription
Despite the benefits of exercise for older adults, several challenges may arise when creating an exercise prescription. Age-related physical limitations, chronic health conditions, and fear of injury can hinder motivation and participation. It is essential to assess an individual’s medical history and current health status before implementing an exercise program. Overcoming barriers such as lack of confidence in abilities or previous negative experiences with physical activity requires a supportive approach. Encouraging positive reinforcement and celebrating small achievements can instill a sense of accomplishment. Additionally, healthcare professionals should work to build rapport with older patients, making them feel comfortable discussing their concerns and preferences. Education about the importance of exercise and addressing misconceptions regarding aging and physical ability can also empower individuals. Moreover, it is vital to collaborate with caregivers or family members to provide additional support where necessary. Introducing modifications in training based on responsiveness to the program and regularly revisiting goals can engage older adults effectively. By addressing these barriers, exercise prescription can be optimized, leading to a more successful and enjoyable experience for older adults seeking to maintain an active lifestyle.
To effectively engage older adults in exercise, creating a supportive environment is vital. Community centers, senior facilities, and rehabilitation centers can play an essential role in promoting physical activity. These locations should include accessible and age-appropriate exercise classes led by qualified instructors who understand the unique needs of older populations. Group activities not only provide social engagement but also enhance motivation, as individuals encourage each other towards achieving their fitness goals. Furthermore, utilizing technology such as fitness trackers or mobile apps can help monitor progress and provide feedback, encouraging adherence to exercise routines. Healthcare professionals must ensure that older adults receive the necessary education regarding safe and effective exercise practices, helping them to understand their bodies and recognize limits. It can also be helpful to include family members or caregivers in the fitness journey, where they can offer support and encouragement. Workshops focusing on health literacy, nutrition, and wellness can further empower older individuals to make informed decisions regarding their health. Ultimately, cultivating a positive exercise culture that prioritizes safety, enjoyment, and community will significantly enhance the effectiveness of exercise prescriptions in older adults.
Types of Exercises for Older Adults
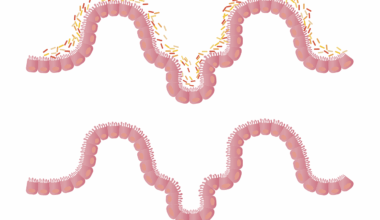
When designing an exercise prescription for older adults, various types of exercises should be incorporated to address different aspects of fitness. A balanced program typically includes aerobic, strength, flexibility, and balance exercises. Aerobic activities, such as brisk walking or low-impact dancing, promote cardiovascular health and enhance endurance. Strength training, utilizing resistance bands or light weights, is crucial for preventing muscle loss and maintaining bone density, which is crucial as individuals age. Flexibility exercises, including stretching routines and yoga, help maintain joint mobility and reduce the risk of injuries. Furthermore, balance exercises such as tai chi or simple stability exercises aid in preventing falls, which is a significant concern for older populations. Each individual may benefit from a distinct combination of these exercise types based on personal health status or physical capability. It is essential that older adults start slowly and progressively increase intensity and duration to avoid overexertion. Additionally, encouraging regular participation in these diverse exercises can help maintain interest and enhance adherence over time. This comprehensive approach to exercise enhances physical fitness and contributes to mental well-being, fostering a healthier aging process.
Incorporating safety measures is paramount when prescribing exercise for older adults. Understanding personal limitations and health conditions is vital in selecting appropriate exercises. Implementing a warm-up and cool-down routine before and after physical activity is highly recommended to minimize the risk of injury and prepare the body for exercise. Moreover, ensuring that the environment is safe, for instance, by eliminating trip hazards and using proper footwear, can further prevent accidents. Regular assessments of physical capability should be performed to identify any necessary modifications in exercises or intensity levels. Additionally, it is essential to stay hydrated, as older adults may have a reduced thirst response, increasing the risk of dehydration during physical activity. Healthcare providers should educate older adults about recognizing signs of overexertion or fatigue, emphasizing the importance of rest and recovery. Coordination with other healthcare providers may help address underlying health issues that can influence exercise capability. Safety should always remain a priority to motivate older adults to engage in regular exercise, enhancing their overall fitness levels and quality of life without the fear of injury or accidents. This approach promotes a sustained and enjoyable physical activity experience.
Long-Term Benefits of Exercise
Engaging in regular exercise has profound long-term benefits for older adults that extend beyond physical capabilities. Studies have shown that consistent physical activity contributes to improved cognitive functions, such as better memory retention and processing speed. Exercise has also been linked to reduced levels of anxiety and depression, providing essential mental health benefits. Furthermore, maintaining an active lifestyle can also contribute to enhanced social connectivity, as participation in group activities provides opportunities for older adults to meet new people and cultivate friendships. Moreover, exercise fosters a sense of purpose and accomplishment that can positively impact overall life satisfaction. In addition to cognitive and emotional benefits, participating in regular physical activity can help manage chronic conditions like arthritis, hypertension, and diabetes, leading to a better quality of life. It is crucial for healthcare professionals to communicate these long-term benefits effectively to encourage ongoing participation. By creating a culture that values fitness and healthy living, older adults are more likely to adopt exercise as a lifelong habit, creating a virtuous cycle of health and wellness that enhances both longevity and life satisfaction.
To successfully promote exercise prescription among older adults, healthcare providers must prioritize comprehensive follow-ups. Regular check-ins can help assess progress, adapt exercise programs, and maintain motivation. These follow-ups should focus on discussing challenges faced, successes achieved, and any changes observed in health status or overall well-being. Tailoring communications based on individual feedback fosters a more personalized approach, critical for sustaining long-term involvement in physical activity. Additionally, using motivational interviewing techniques can help address ambivalence towards exercise, encouraging individuals to articulate their personal goals. Providing resources, such as educational materials and referrals to fitness programs, enhances accountability and supports continued activity. Furthermore, partnering with community resources, like fitness instructors specializing in senior fitness, expands options available to older adults. Creating a support network including family, friends, or significant others can positively influence adherence to exercise plans by providing encouragement. Ultimately, these continuous support mechanisms facilitate a consistent exercise routine, enabling older adults to reap long-lasting benefits, bolstering their health, happiness, and overall quality of life.
In conclusion, exercise prescription for older adults presents numerous strategies and benefits tailored to meet the unique challenges faced by this population. By incorporating various types of exercises and ensuring safety during physical activity, healthcare providers can significantly enhance older adults’ overall health and quality of life. Emphasizing the importance of a supportive environment and community resources is crucial for fostering adherence and motivation. Moreover, understanding the long-term benefits of regular exercise can inspire continuous participation, leading to improved physical, mental, and social well-being. Tailoring exercise programs to accommodate individual preferences and limitations allows for a more inclusive approach, promoting adherence and enjoyment. Additionally, effective follow-up strategies are necessary to maintain engagement trajectories and optimize program outcomes. As more healthcare professionals recognize the vital role of exercise in aging populations, the development and implementation of individualized exercise prescriptions will become increasingly prioritized. This approach not only mitigates health risks associated with inactivity but also ensures that older adults can maintain a vibrant and fulfilling lifestyle as they age. Ultimately, promoting active living among seniors is integral to enhancing their overall health and promoting independence.