Meal Planning for Exercise Recovery Following Hypoglycemia
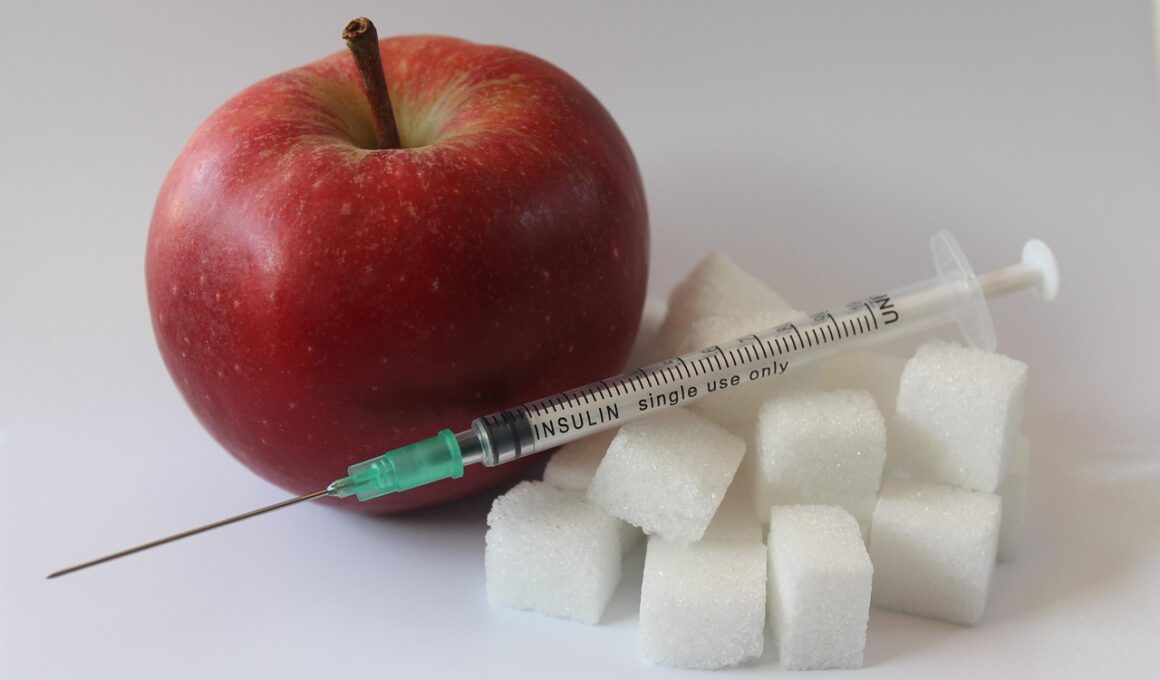
After experiencing a hypoglycemic episode, proper recovery becomes an essential aspect of managing diabetes effectively. This recovery involves not just monitoring blood sugar levels, but also planning meals that support an optimal recovery process. Consuming carbohydrates is particularly vital, as they directly replenish depleted glucose levels in the bloodstream. Ensuring that these carbohydrates come from quality sources is just as crucial, as whole grains and fruits provide essential nutrients and fiber. In this context, balanced meal planning means considering proteins and healthy fats alongside carbohydrates to create a well-rounded post-exercise meal. Lean meat, legumes, and nuts are excellent additions that can stabilize blood sugar. It is advisable to consume a meal or snack that includes these components within 30 minutes post-exercise. This time frame allows for effective recovery while also preventing potential dips in blood sugar. It is equally important to stay hydrated, as fluids can support overall bodily functions. Remember, effective meal planning is crucial, not only for immediate recovery but also for sustaining long-term health and fitness goals. Consider working closely with healthcare professionals for personalized guidance on diet and exercise routines.
A Balanced Approach to Recovering Post-Hypoglycemia
The significance of meal planning after a hypoglycemic episode can’t be understated. It not only aids in immediate recovery but also influences long-term lifestyle habits. Start by identifying the duration of the exercise, which can help tailor your carbohydrate intake to replenish energy stores adequately. For instance, high-intensity workouts typically lead to a greater depletion of glycogen stores, necessitating a more substantial carbohydrate intake post-exercise. Moreover, pre-planning meals can help prevent panic or confusion when craving food after hypoglycemia. Prepare nutrient-dense snacks or meals in advance so they are ready to consume. Selecting options low in glycemic index can assist in avoiding spikes and subsequent crashes in blood sugar levels. Whole foods, including grains, legumes, and fresh produce, are generally more effective than processed snacks. As important as food is, recognizing one’s body’s signals is invaluable. Keeping a food diary can help track what works best for individual recovery experiences. This practice assists in developing effective patterns of eating that align with exercise and blood sugar levels. Encourage patients to discover food combinations that yield favorable outcomes, enhancing their overall healthy lifestyle.
After hypoglycemic incidents, restorative meals should emphasize easily digestible carbohydrates that provide quick energy. Options such as bananas, whole-grain bread, and yogurt can work effectively. Pairing these with protein sources will improve recovery further. For instance, a banana with a handful of nuts or yogurt can offer that balance. While food is critical, hydration significantly contributes to recovery as well. Water is the optimal choice. Avoid excessively sweet or sugary drinks, as they may create another spike in blood sugar, which could lead to another crash later. Increasing the intake of vegetables post-exercise ensures the body receives the vitamins and minerals necessary during recovery. Leafy greens, bell peppers, and squash are nutrient-dense and offer electrolytes. Adjusting meal portions based on exercise intensity or frequency is also essential; more demanding workouts may require increased calorie intake. This principle helps maintain stable blood sugar levels, leading to improved performance and easier exercise management. Overall, thoughtful meal planning paired with monitoring can facilitate better recovery and minimize hypoglycemic incidences. Individuals should remember that success in maintaining blood sugar levels involves a harmony of foods, exercise, and rest.
Timing of Carbohydrate Consumption
Timing when carbohydrates are consumed plays an influential role in recovery following exercise and hypoglycemic episodes. Consuming carbohydrates ideally within 30 minutes post-exercise significantly speeds up recovery. This timeframe is crucial because it’s often referred to as the “anabolic window,” a period during which your body is particularly responsive to nutrients. Eating quickly after exertion can reduce muscle breakdown and enhance glycogen synthesis, which is essential for individuals with diabetes. Keep in mind that rapid recovery can minimize the risk of future hypoglycemic events. Snack ideas could include a peanut butter sandwich on whole-grain bread or a smoothie containing spinach, fruits, and protein powder. Combining carbohydrates with protein can further support muscle recovery. Experimenting with before and after meals can help you find a routine that relieves anxiety surrounding hypoglycemia. Resources such as [American Diabetes Association](https://www.diabetes.org) provide exemplary meal plans and support, enabling individuals to make informed choices. The combination of good nutrition and thoughtful meal timing not only improves recovery but also encourages effective diabetes management, illustrating the direct link between food, exercise, and overall well-being.
A vital aspect of meal planning is also considering the day-to-day lifestyle of individuals. Understanding that daily routines can vary significantly influences what types of meals are practical. Working professionals or busy parents may benefit from quick, nutrient-rich meals that can be prepared in advance. Batch cooking is an effective strategy, allowing individuals to prepare several meals or snacks in one cooking session, saving time during busy weekdays. Incorporate ingredients that not only support recovery but also fulfill personal preferences to enhance the overall experience. It is equally important not to overlook emotional well-being. Food can be a source of comfort, and balancing it with health benefits can create a more positive relationship with meals. Allowing occasional indulgences, as long as they fit within the broader recovery plan, fosters sustainability in nutrition habits. Awareness of one’s nutritional goals accentuates motivation and commitment to a diabetes management plan. As a result, structured meal planning can yield rewarding outcomes while establishing consistency in routine and execution, ultimately making the journey towards health more manageable. Keeping in mind personal preferences ensures a more enjoyable recovery experience.
Utilizing Technology for Meal Planning
In today’s digital age, utilizing technology for meal planning is a game-changer for diabetes management. Numerous mobile applications exist to assist with tracking meals, monitoring carbohydrate intake, and suggesting recipes. These tools can simplify the process and help individuals stay accountable to their meal plans. They can enable users to scan barcodes of foods, ensuring accurate carbohydrate counts while saving valuable time. This technology can also be integrated with blood glucose monitoring devices, allowing for a seamless record of how certain foods affect glucose levels post-exercise. Besides, logging meals and snacks yields insights over time, helping identify steady meal patterns conducive to maintaining balanced blood sugar levels. Participating in online communities can also serve as a source of support, providing members with shared experiences and meal suggestions. Exchange recipes, learn about new healthy food alternatives, and create meal plans through virtual platforms. Staying informed on the latest nutrition research via reputable health blogs can help ensure meal plans are not only enjoyable but also effective. Emphasizing technology in meal planning promotes empowerment among those living with diabetes, leading to a more active and engaged lifestyle, reducing stress around managing their condition.
Lastly, ongoing education and support systems are crucial for ensuring effective meal planning that supports recovery after hypoglycemia. Partnering with dietitians and diabetes educators provides access to personalized advice tailored to individuals’ unique needs. Consultations create opportunities for individuals to discuss their experiences, challenges, and successes. Encouraging active participation in workshops or seminars can also foster a sense of community. Engaging with peers who face similar circumstances can provide different perspectives and coping strategies. Sharing experiences helps mitigate feelings of isolation that can accompany chronic conditions. Local diabetes organizations might offer resources and connections to nutrition education classes. These classes enhance indispensable skills for managing daily diabetes routines. Empowerment through education fosters independence and confidence when it comes to making food choices. As a result, lasting health and fitness goals can be achieved. Incorporating all the aspects mentioned, meal planning serves as a cornerstone in the recovery journey following hypoglycemic episodes. Encourage open dialogue with healthcare professionals, technology utilization, and ongoing education to create a supportive environment. This framework ultimately contributes to a balanced, healthy lifestyle, making diabetes management a more rewarding and manageable endeavor.