Intermittent Fasting and Gut Microbiome Changes in Diabetic Individuals
Intermittent fasting (IF) has gained significant attention for its potential health benefits, particularly for individuals with diabetes. The practice involves cycling between eating periods and fasting intervals, impacting insulin sensitivity and glucose metabolism. Research indicates that IF may alter gut microbiota composition, which plays a crucial role in metabolism and is particularly relevant for diabetic patients. Several studies suggest that fasting can lead to favorable shifts in gut bacteria, promoting species that enhance metabolic health and reduce inflammation. Additionally, these changes may improve barrier function, reducing the risk of complications. Those with diabetes might benefit from adopting IF, as it not only aids glucose control but also positively influences gut health. This connection between fasting and microbiome diversity could unlock new strategies for managing diabetes. Overall, the interplay between IF and gut microbiota signifies a promising area for further exploration. Future research should focus on understanding specific bacterial strains affected by IF and their roles in glycemic control, inflammation reduction, and overall metabolic health in diabetic individuals. This could pave the way for more personalized dietary recommendations based on individual microbiome profiles.
One significant aspect of intermittent fasting is its timing and structure, which greatly affects the efficacy of the practice. Various methods of IF exist, including the 16/8 method, the 5:2 diet, and alternate-day fasting. Each method presents unique benefits and challenges for individuals with diabetes. The 16/8 method, which allows an eating window of eight hours followed by a sixteen-hour fast, is particularly popular due to its simplicity and ease of incorporation into daily routines. Research has shown that adhering to this protocol can lead to improved blood sugar levels and reduced insulin resistance. However, individuals must remain cautious and monitor their blood glucose levels diligently during fasting periods. The 5:2 diet, characterized by normal eating for five days and caloric restriction for two non-consecutive days, may also be effective for some. It is crucial to emphasize a balanced diet during eating windows to ensure adequate nutrient intake. Emphasizing fiber-rich foods, lean proteins, and healthy fats can promote satiety and metabolic health, making intermittent fasting a viable strategy for better diabetes management.
Gut Microbiome’s Role in Diabetes
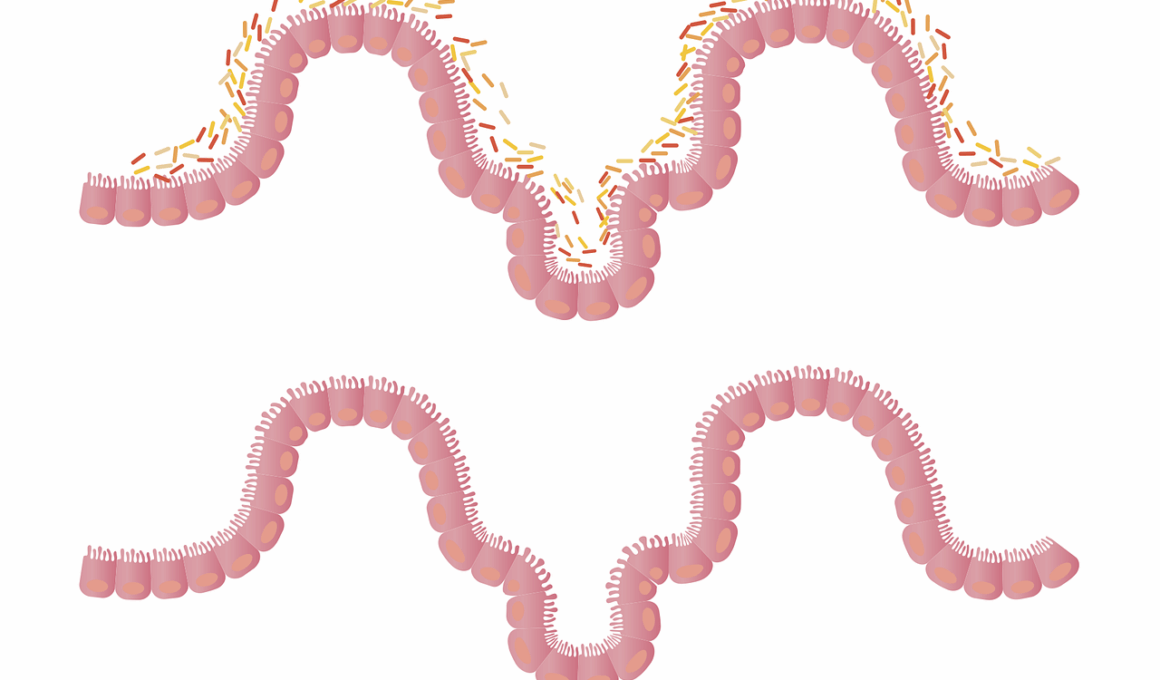
The gut microbiome influences several aspects of health, encompassing digestion, metabolism, and immune function. In diabetic individuals, an imbalance in gut bacteria has been linked to insulin resistance and inflammation. Specific bacterial species are known to affect the absorption of nutrients and the production of short-chain fatty acids (SCFAs), which play a pivotal role in metabolic processes. Beneficial gut bacteria help modulate glucose metabolism and enhance the body’s ability to respond to insulin effectively. Intermittent fasting could help recalibrate gut microbiota composition, thereby improving the quality and diversity of beneficial bacteria. This shift may result in improved blood sugar control, reduced systemic inflammation, and a lower risk of complications associated with diabetes. Studies have shown that individuals following IF experience increased levels of SCFAs, particularly butyrate, which has therapeutic potential in sugar metabolism and inflammation reduction. Understanding the specific mechanisms through which IF influences gut microbiota will be essential for future therapeutic approaches in managing diabetes and improving overall health outcomes for affected individuals.
Implementing intermittent fasting among those with diabetes requires careful consideration and individualized strategies. Medical professionals should evaluate patient health status, diabetic complications, and lifestyle factors before recommending any fasting regimen. In addition, education regarding signs of hypoglycemia during fasting is crucial. Patients should learn how to adjust medication and monitor blood sugar levels effectively. It is essential to establish a supportive framework for those transitioning to IF. Support groups, advice from healthcare providers, and resources on meal planning can ease the process. Developing a balanced diet emphasizing whole foods rich in nutrients will ensure optimal metabolic function during eating periods. Additionally, gradual integration of fasting protocols may help diabetic individuals adapt effectively. Assessing personal comfort levels with fasting durations is vital to encourage sustainability. Implementing intermittent fasting shouldn’t compromise medication adherence, regular check-ups, and healthy lifestyle habits such as exercise. Through comprehensive support and education, individuals can harness the benefits of intermittent fasting while managing diabetes successfully. The synergy between IF and enhanced gut health may lead to improved diabetes outcomes in the long term.
Potential Benefits of Intermittent Fasting
The potential benefits of intermittent fasting for diabetic individuals extend beyond glycemic control and gut microbiota modulation. Fasting can also promote weight loss by inducing a caloric deficit, which is often crucial for managing type 2 diabetes. Losing weight may improve insulin sensitivity and contribute to overall metabolic health. Additionally, intermittent fasting has been linked to reduced oxidative stress and inflammation, which are risk factors common among diabetic patients. The period without food intake allows the body to undergo various adaptive processes, such as autophagy, which may help eliminate damaged cells and contribute to improved cellular health. Fasting activates cellular repair mechanisms and promotes hormone regulation, aiding in better metabolic signaling. Furthermore, intermittent fasting can influence mental clarity and energy levels. Many individuals report enhanced focus and productivity during fasting periods, possibly due to stabilized blood sugar levels. Exploring these multifaceted benefits may lead to more comprehensive approaches for managing diabetes and achieving sustainable health improvements. As research evolves, understanding how fasting influences overall wellbeing will be vital for formulating effective treatment strategies.
As we delve deeper into the relationship between intermittent fasting and diabetes, it is essential to highlight the need for ongoing research. Despite promising findings, much remains to be understood about the exact mechanisms by which fasting influences gut microbiota composition and, subsequently, metabolic outcomes. Large-scale clinical trials and observational studies will be necessary to validate initial findings and establish standardized fasting protocols. Researchers should focus on identifying specific bacterial strains, their functions, and how their shifts during chronological fasting periods correlate with improvements in diabetes management. Investigating the impact of lifestyle factors, such as diet and physical activity, alongside intermittent fasting will further elucidate their roles in optimizing gut health. Additionally, understanding individual variations in microbiome responses to fasting will be paramount for personalization of such dietary strategies. Emphasizing collaboration between nutritionists, healthcare providers, and researchers will ensure comprehensive insights into the benefits and challenges associated with intermittent fasting in diabetic populations. Continuous education and awareness within clinical environments, along with patient support, will also contribute to effective implementations of intermittent fasting as a meal strategy for managing diabetes.
Conclusion
In conclusion, intermittent fasting shows promise as an effective strategy for managing diabetes, particularly regarding gut microbiome alterations. These changes in microbiota can play an essential role in improving metabolic health and enhancing overall wellbeing in diabetic individuals. While many benefits arise from fasting, such as weight management, improved insulin sensitivity, and reduced inflammation, careful implementation and individualized approaches remain crucial. Patients considering intermittent fasting should prioritize monitoring blood sugar levels, adhering to medication regimens, and obtaining guidance from healthcare professionals. Future research will provide further clarity on the interplay between intermittent fasting, gut microbiota, and diabetes management. Understanding these connections opens up opportunities for personalized dietary approaches aimed at maximizing health outcomes for those struggling with diabetes. Ongoing exploration into gut health’s role in metabolic diseases underscores its significance in disease prevention and management. As knowledge advances, intermittent fasting may evolve into a mainstream recommendation for diabetes care. Comprehensive understanding and collaborative efforts between various stakeholders will bolster the effectiveness of these dietary strategies, ensuring healthier lifestyles for individuals living with diabetes.
In summary, intermittent fasting represents a compelling area of research within the diabetes management landscape. The evolving understanding of the interplay between fasting and gut microbiota brings new insights into dietary strategies. Practitioners should remain informed about evidence-based benefits and challenges associated with intermittent fasting among diabetic populations. Establishing a clear communication pathway between healthcare providers and patients will facilitate the safe adoption of fasting protocols. As the body of research expands, the essential connections between lifestyle interventions and metabolic health will inspire innovative therapeutic modalities. Fostering an environment of support and encouragement is vital for patient engagement in adopting intermittent fasting. The positive implications of gut microbiome modulation on health outcomes provide a foundation for ongoing exploration. Intermittent fasting could ultimately pave the way for a transformative approach to managing diabetes that prioritizes metabolic health and well-being. Empowering patients with knowledge and tools to navigate fasting successfully can enhance their quality of life and achieve better health outcomes.