Intermittent Fasting as a Strategy to Manage Insulin Resistance
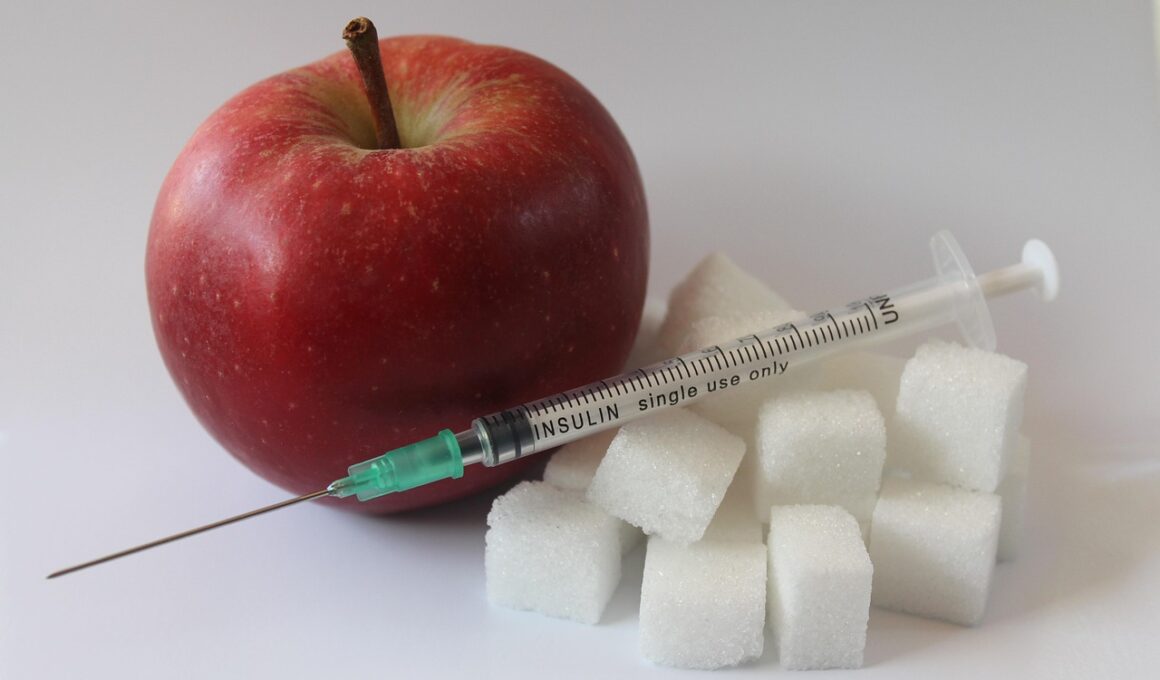
Intermittent fasting (IF) is gaining attention as a potential approach for managing insulin resistance. This metabolic condition occurs when the body’s cells become less responsive to insulin, leading to elevated blood sugar levels. One widely recognized benefit of intermittent fasting is its influence on insulin levels within the bloodstream. By restricting food intake to specific periods, IF can aid in lowering overall insulin levels, which is crucial for those with insulin resistance. Additionally, various studies have found that regular practice of intermittent fasting can enhance insulin sensitivity. This means the body becomes more efficient at using insulin, potentially reversing negative metabolic conditions associated with diabetes. Moreover, intermittent fasting may lead to weight loss, creating a dual benefit when paired with dietary restrictions. When individuals lose weight through caloric restriction and structured eating patterns of IF, insulin sensitivity generally improves. It’s vital, however, to approach intermittent fasting cautiously and consult healthcare professionals particularly for individuals with existing health conditions. Combing fasting with a balanced diet ensures not only reduced insulin levels but also holistic wellness and health improvement. Thus, understanding IF’s impact on insulin resistance is crucial for optimal health.
The effects of intermittent fasting on insulin resistance extend beyond mere weight loss. When individuals engage in fasting, there is a notable reduction in insulin secretion by the pancreas. This decrease results from periods of fasting, allowing insulin levels to remain low during fasting intervals. This mechanism supports cellular efficiency and the body’s overall energy regulation. Additionally, intermittent fasting is associated with increased fat oxidization as the body relies on fat stores for energy when glucose is limited during fasting. This metabolic shift can further improve insulin sensitivity, creating a more favorable environment for glucose processing. Research has shown that intermittent fasting can lead to significant improvements in blood sugar levels and glycemic control, which are essential for managing insulin resistance. Furthermore, by increasing the body’s ketone levels, intermittent fasting can enhance mitochondrial efficiency and overall metabolic health. Regular fasting periods encourage adipose tissue health and help to modulate inflammation, factors that significantly contribute to insulin resistance. Therefore, understanding these dual benefits—improved insulin sensitivity and reduced inflammation—positions intermittent fasting as a powerful strategy against insulin resistance.
Incorporating intermittent fasting into one’s lifestyle is not just about timing; it involves choosing the right approach. Numerous methods of intermittent fasting exist, such as the 16/8 method, where individuals fast for 16 hours and eat during an 8-hour window. Another effective approach is the 5:2 method, which restricts calorie intake for two days of the week while maintaining normal eating on other days. These methods can be adapted depending on individual preferences and schedules. It is important to select a fasting regimen that suits your lifestyle, as adherence plays a crucial role in the benefits gained. Additionally, focusing on nutrient-dense foods during eating windows helps maintain energy levels and provides necessary vitamins and minerals to support bodily functions. For optimal results, individuals should incorporate whole foods, plenty of vegetables, lean proteins, and healthy fats into their meals. Equally important is to stay hydrated, as dehydration can cause cravings and diminish the benefits of fasting. By adopting a structured approach, one can maximize the health benefits of intermittent fasting, particularly its effects on managing insulin resistance.
Challenges of Intermittent Fasting can arise during the initial stages of adaptation to this eating schedule. Individuals may experience hunger pangs, mood swings, or irritability as their bodies adjust to a new eating pattern. However, these symptoms typically diminish within the first week of consistently practicing intermittent fasting. Generally, fasting stimulates autophagy, a process where the body cleans out damaged cells and regenerates newer, healthier cells, further supporting metabolic health. Moreover, seeking support from online communities or local groups can enhance motivation and encourage adherence to the fasting routine. Engaging with others promotes shared experiences and helpful tips that can ease the transition. Tracking progress, whether through body measurements or blood sugar logs, can provide motivation and highlight the benefits achieved. Furthermore, making small adjustments to eating windows can accommodate busy lifestyles, ensuring that intermittent fasting remains feasible and enjoyable. Thus, although challenges exist, understanding these obstacles can help individuals persevere and reap the benefits associated with improved insulin sensitivity through intermittent fasting.
Long-Term Effects of IF on Insulin Resistance
The long-term effects of intermittent fasting on insulin resistance are noteworthy and merit comprehensive exploration. Studies have suggested that sustained intermittent fasting can lead to lasting improvements in not only insulin sensitivity but also overall metabolic health. Individuals practicing intermittent fasting over extended periods reported greater control over blood sugar levels, leading to a marked decrease in the need for medication in some cases. Here, the synergy between fasting and consistent lifestyle choices, such as regular physical activity and balanced nutrition, amplifies these benefits. Moreover, intermittent fasting may promote longevity by reducing the risk factors associated with chronic diseases linked to insulin resistance, such as heart disease and type 2 diabetes. The reduction of visceral fat is also a prominent benefit, as this type of fat is closely tied to insulin resistance. If individuals maintain a fasting schedule alongside healthy eating habits, they may significantly reduce their risk for metabolic syndrome. Overall, the positive long-term implications of intermittent fasting provide compelling reasons to consider this dietary approach for managing insulin resistance.
As with any dietary strategy, personal consistency and commitment are essential for effectiveness. Tracking dietary habits can assist in understanding patterns and ensuring that fasting integrates seamlessly with one’s daily routine. It is equally vital to remain flexible and adjust fasting windows according to lifestyle changes using personal judgement. For instance, if significant commitments arise, slight alterations to the fasting schedule can maintain overall health progress. Furthermore, considering an individual’s mental relationship with food is crucial; positive reinforcement aids in fostering a healthy attitude toward nutrition. In addition, collaborating with healthcare professionals for an individualized plan can ensure that the implementation of intermittent fasting meets specific goals and monitoring health outcomes effectively. A tailored approach recognizes that each individual’s body responds uniquely to intermittent fasting and may necessitate adjustments. Educating oneself about the biological processes occurring during fasting yields insights, enhancing comprehension and appreciation for the journey toward improved insulin sensitivity. Therefore, building a personal connection to intermittent fasting signals a commitment to achieving greater health.
Conclusion
In conclusion, intermittent fasting emerges as a promising strategy for improving insulin resistance. Its ability to lower insulin levels and enhance insulin sensitivity presents substantial benefits for those with metabolic disorders. Practicing intermittent fasting can lead to weight loss and better blood sugar control, serving as a dual focal point for combating insulin resistance. Studies underline the long-term advantages of intermittent fasting and its collaborative role in a comprehensive lifestyle approach, including exercise and proper nutrition. Integrating fasting with healthy eating supports sustainable results necessary for managing insulin resistance effectively. While challenges may arise, the adaptability of intermittent fasting can accommodate individual preferences and needs. For long-lasting benefits, commitment to this fasting approach must align with personal lifestyle modifications and overall wellness goals. Staying informed, patient, and persistent makes the journey towards better health successful. Ultimately, with an informed perspective and supportive environment, individuals can harness the power of intermittent fasting to manage insulin resistance effectively. Exploring fasting not only impacts physical health positively but can also enrich one’s overall quality of life.
Adopting intermittent fasting aligns with current health trends aiming to combat rising obesity and diabetes rates. Individuals can cultivate a healthier relationship with food while potentially enhancing overall well-being and longevity. In research, sustained intermittent fasting has shown to extend lifespan in various models. Thus, familiarizing oneself with the multifaceted approaches of intermittent fasting solidifies its place as a valuable asset in managing insulin resistance and overall health. Optimizing the fasting experience means focusing on well-rounded dietary choices and consistent habits. Finding a supportive community can significantly amplify motivation and success.